Key Takeaways
- The study analyzed over 22,000 prostate cancer patients, revealing a growing prevalence of localized and locally advanced cases.
- Clinical outcomes varied significantly by treatment type, with radiotherapy and radical prostatectomy showing the highest survival rates.
- Increased age and comorbidities were linked to poorer treatment responses and survival outcomes among patients receiving androgen deprivation therapy.
Prostate Cancer Patient Overview
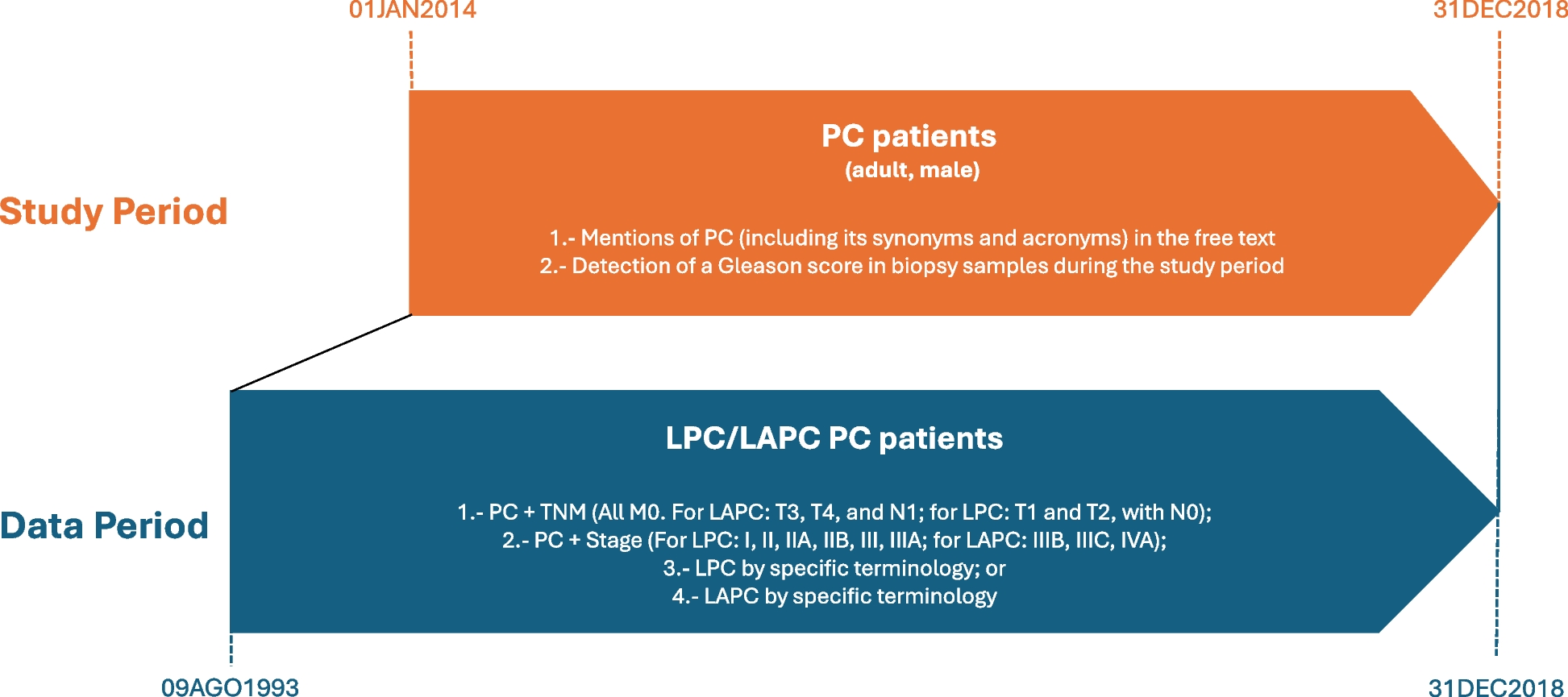
A comprehensive study investigated the demographics and clinical characteristics of 22,166 prostate cancer (PC) patients from a larger pool of 2,626,612 individuals treated at participating hospitals. Among these patients, 65.1% were classified as having localized or locally advanced prostate cancer (LPC/LAPC), with increasing prevalence observed from 729.1 per 100,000 persons in 2014 to 895 in 2018. The incidence rate, however, declined from 123.3 to 91.9 per 100,000 during the same period.
The population’s median age at diagnosis was 68 years, and 14.5% had a family history of PC. Common comorbidities included hypertension (41.6%) and hypercholesterolemia (28.2%). A significant portion of patients (67.8%) were asymptomatic, prompting a closer look at treatment modalities. The initial treatment varied, with 40.7% receiving radiotherapy (RT), 37.1% undergoing radical prostatectomy (RP), and 6.4% on active surveillance.
Among the treatment groups, patients starting with androgen deprivation therapy (ADT) were typically older, displayed higher rates of comorbidities, and had elevated median PSA levels (13.4 ng/mL). Healthcare utilization revealed that 92.5% attended at least one outpatient visit, while hospitalization rates were notably higher among those treated with brachytherapy or RP.
Clinical Outcomes and Survival Rates
The estimated median follow-up for all LPC/LAPC patients was approximately 4.1 years. Although exact median overall survival (OS) and metastasis-free survival (MFS) rates have not been reached, event-free survival (EFS) was 33.7 months. Results indicated that clinical outcomes worsened as risk increased: 91% OS at 36 months for LAPC patients compared to 98% for low-risk LPC patients.
Patients were stratified by initial treatment received, showing substantial variations in OS and EFS. For example, the ADT-only group had the lowest OS rate at 79% at 36 months, while both RT and RP patients demonstrated significantly higher rates nearing 98%. Furthermore, the ADT group experienced the highest percentage of metastasis development during the follow-up.
Thus, this study underscores the critical importance of patient demographics and treatment choices in determining clinical outcomes for prostate cancer, highlighting significant disparities in survival based on the type of therapy received and patient health factors.
The content above is a summary. For more details, see the source article.